HISTORY OF HOMEOPATHY
The theories and principles of homeopathy have their origins in medicinal traditions established thousands of years ago in Ancient Greece and Rome.
In the 5th century BCE the Greek physician Hippocrates (460–377 BCE) clearly established the idea that disease was the result of natural forces rather than divine intervention, and that patients’ own powers of healing should be encouraged (see page 19). Contemporary medical theories were based upon the Law of Contraries, which advocated treating an illness by prescribing a substance that produced opposite or contrary symptoms. Diarrhea, for example, could be treated by a substance that caused constipation, such as aluminum hydroxide.
In contrast, Hippocrates developed the use of the Law of Similars, based on the principle that “like cures like” (see page 18). This theory proposed that substances capable of causing symptoms of illness in healthy people could also be used to treat similar symptoms during illness. For example, Veratrum album (white hellebore), which was considered effective against cholera, caused violent purging that led to severe dehydration if administered in large doses—symptoms exactly like those of cholera itself. Between the 1st and 5th centuries CE the Romans made further developments in medicine. They introduced more herbs into the pharmacopeias, improved public hygiene, and observed the structure and function of the human body, although this was limited by social taboo, which prevented the dissection of bodies. Existing medical knowledge was codified and rationalized by Galen (130–200 CE), a Roman physician, anatomist, and physiologist.
He adopted many ancient Greek principles, including the Aristotelian theory o the “four humors,” which claimed that the human body was made up of four humors—blood, choler (yellow bile), melancholy (black bile), and phlegm— that must be kept in balance to ensure vitality and health.
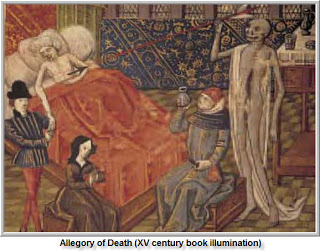
After the decline of the Roman empire, little progress was made for centuries in the field of European medicine. A combination of herbal folklore, religious influences, and Galenic theory provided the basis for understanding and treating illness right through to the 17th century. Only when the Swiss physician and alchemist Paracelsus (1493–1541) began to develop his theories did the study of medicine start to evolve again. Paracelsus revived the ancient Greek theory of the Doctrine of Signatures, which was based on the premise that the external appearance of a plant—God’s “signature”—indicated the nature of its healing properties. For example,Chelidonium majus (greater celandine) was used to treat conditions affecting the liver and gallbladder because the yellow juice of the plant resembled bile.
Paracelsus argued that disease was linked to external factors such as contaminated food and water rather than to mystical forces, and he challenged his contemporaries to recognize the body’s natural ability to heal itself, claiming that the practice of medicine should be based on detailed observation and “profound knowledge of nature and her works.” According to his theories, all plants and metals contained active ingredients that could be prescribed to match specific illnesses. Concentrating on practical experiments rather than on alchemy, he laid the foundations for the early stages of chemistry and subsequent development of pharmaceutical medicine, introducing new medicines, such as opium, sulfur, iron, and arsenic, into the contemporary repertory. His exploration of the chemical and medicinal properties of many substances, and his advocacy of the Hippocratic concept of “like cures like,” also made Paracelsus a key figure in the development of homeopathy.
According to the British homeopath James Compton Bunett (1840–1901), the author of several important works on homeopathy that are still in use today, “Paracelsus planted the acorn from which the mighty oak of homeopathy has grown.” intellectual climate encouraged important developments in the study of medicine, including the isolation of active ingredients from herbs, such as the extraction of morphine from the opium poppy in 1803. It was in 1790, while translating A Treatise on Materia Medica by a Scottish teacher, physician, and chemist, Dr. William Cullen, that Hahnemann began an investigation which was to prove paramount to the subsequent development of homeopathy. In his treatise Cullen argued that quinine, when isolated from Cinchona officinalis (see page 49), was a good treatment for malaria because it was an stringent. Hahnemann knew that other, more powerful, astringents had no such effect on malaria.
He dosed himself with quinine, recording the results and effectively beginning the first “proving” see page 22). Although he did not have malaria, he found that he began to develop symptoms of the disease one after the other. With each dose of quinine, the symptoms recurred and lasted for several hours, but if he stopped taking quinine his symptoms began to disappear. Hahnemann went on to test quinine on other people, noting their reactions in great detail. The test subjects were not allowed to eat or drink strong foods such as spices, alcohol, or coffee, which he felt might distort the results. He repeated the proving process on other substances that were in use as medicines, such as arsenic and belladonna, and used the results to build up a “symptom picture” of each remedy’s effects (see page 23).
After conducting provings for six years, Hahnemann extended his research to the sick. Prior to prescription, he gave his patients a thorough physical examination and noted any existing symptoms. He questioned them closely regarding their lifestyles, general health, outlook on life, and other factors that made them feel better or worse. Following the principle of like cures like, Hahnemann then matched individual symptoms as closely as possible to the symptom picture of a remedy, and prescribed accordingly.
In contrast, Hippocrates developed the use of the Law of Similars, based on the principle that “like cures like” (see page 18). This theory proposed that substances capable of causing symptoms of illness in healthy people could also be used to treat similar symptoms during illness. For example, Veratrum album (white hellebore), which was considered effective against cholera, caused violent purging that led to severe dehydration if administered in large doses—symptoms exactly like those of cholera itself. Between the 1st and 5th centuries CE the Romans made further developments in medicine. They introduced more herbs into the pharmacopeias, improved public hygiene, and observed the structure and function of the human body, although this was limited by social taboo, which prevented the dissection of bodies. Existing medical knowledge was codified and rationalized by Galen (130–200 CE), a Roman physician, anatomist, and physiologist.
He adopted many ancient Greek principles, including the Aristotelian theory o the “four humors,” which claimed that the human body was made up of four humors—blood, choler (yellow bile), melancholy (black bile), and phlegm— that must be kept in balance to ensure vitality and health.
After the decline of the Roman empire, little progress was made for centuries in the field of European medicine. A combination of herbal folklore, religious influences, and Galenic theory provided the basis for understanding and treating illness right through to the 17th century. Only when the Swiss physician and alchemist Paracelsus (1493–1541) began to develop his theories did the study of medicine start to evolve again. Paracelsus revived the ancient Greek theory of the Doctrine of Signatures, which was based on the premise that the external appearance of a plant—God’s “signature”—indicated the nature of its healing properties. For example,Chelidonium majus (greater celandine) was used to treat conditions affecting the liver and gallbladder because the yellow juice of the plant resembled bile.
Paracelsus argued that disease was linked to external factors such as contaminated food and water rather than to mystical forces, and he challenged his contemporaries to recognize the body’s natural ability to heal itself, claiming that the practice of medicine should be based on detailed observation and “profound knowledge of nature and her works.” According to his theories, all plants and metals contained active ingredients that could be prescribed to match specific illnesses. Concentrating on practical experiments rather than on alchemy, he laid the foundations for the early stages of chemistry and subsequent development of pharmaceutical medicine, introducing new medicines, such as opium, sulfur, iron, and arsenic, into the contemporary repertory. His exploration of the chemical and medicinal properties of many substances, and his advocacy of the Hippocratic concept of “like cures like,” also made Paracelsus a key figure in the development of homeopathy.
According to the British homeopath James Compton Bunett (1840–1901), the author of several important works on homeopathy that are still in use today, “Paracelsus planted the acorn from which the mighty oak of homeopathy has grown.” intellectual climate encouraged important developments in the study of medicine, including the isolation of active ingredients from herbs, such as the extraction of morphine from the opium poppy in 1803. It was in 1790, while translating A Treatise on Materia Medica by a Scottish teacher, physician, and chemist, Dr. William Cullen, that Hahnemann began an investigation which was to prove paramount to the subsequent development of homeopathy. In his treatise Cullen argued that quinine, when isolated from Cinchona officinalis (see page 49), was a good treatment for malaria because it was an stringent. Hahnemann knew that other, more powerful, astringents had no such effect on malaria.
He dosed himself with quinine, recording the results and effectively beginning the first “proving” see page 22). Although he did not have malaria, he found that he began to develop symptoms of the disease one after the other. With each dose of quinine, the symptoms recurred and lasted for several hours, but if he stopped taking quinine his symptoms began to disappear. Hahnemann went on to test quinine on other people, noting their reactions in great detail. The test subjects were not allowed to eat or drink strong foods such as spices, alcohol, or coffee, which he felt might distort the results. He repeated the proving process on other substances that were in use as medicines, such as arsenic and belladonna, and used the results to build up a “symptom picture” of each remedy’s effects (see page 23).
After conducting provings for six years, Hahnemann extended his research to the sick. Prior to prescription, he gave his patients a thorough physical examination and noted any existing symptoms. He questioned them closely regarding their lifestyles, general health, outlook on life, and other factors that made them feel better or worse. Following the principle of like cures like, Hahnemann then matched individual symptoms as closely as possible to the symptom picture of a remedy, and prescribed accordingly.
Development & definition
Hahnemann’s work gradually brought about the establishment of new type of medicine. In 1796 he published his first book on the subject, entitled A New Principle for Ascertaining the Curative Powers of Drugs and Some Examinations of Previous Principles. He called his new system “homeopathy,” from the Greek homeo meaning “similar” and pathos meaning “suffering.” In 1810 he set out its principles in The Organon of Rationale Medicine, and two years later he began teaching homeopathy at the University of Leipzig. During the course of his lifetime, Hahnemann proved about 100 remedies, and also continued to develop and refine the theory and practice of the system (see page 18).
The medical establishment remained generally very sceptical of Hahnemann’s theories, and he in turn continued to be intensely critical of conventional medical practice. He became known as the “raging hurricane” due to his furious tirades and sarcastic critiques during lectures at Leipzig. He also antagonized contemporary pharmacists by giving only one medicine at a time, which was contrary to their (highly lucrative) practice of generally prescribing expensive mixtures of several remedies. During the 19th century, homeopathy spread rapidly across Europe to Asia and the Americas. In the US, Dr. Constantine Hering (1800–80) and Dr. James Tyler Kent (1849–1916) were responsible for popularizing the therapy and introducing new ideas and practices (see page 19). By the time of Hahnemann’s death in 1843, homeopathy was firmly established in many parts of the world, although there remained antagonism and distrust between the advocates of conventional medicine and those of homeopathy.
Between 1860 and 1890 homeopathy flourished, as many homeopathic hospitals and schools were opened, and many new remedies were proved, considerably enlarging the materia medica. Hahnemann’s followers were often doctors who defected from conventional medicine after personally experiencing treatment, including an English doctor, Frederick Quin (1799–1878), who was cured of cholera by the Camphora remedy. Quin first visited Hahnemann in Germany in 1826, and went on to introduce homeopathy in the UK, founding the first homeopathic hospital in London in 1849. During a cholera outbreak in 1854, the mortality rate at his hospital was less than half that of conventional hospitals. This information was suppressed by the national Board of Health on the grounds that “the figures would give sanction to a practice opposed to the maintenance of truth and the progress of science,” illustrating the close stranglehold the medical establishment had achieved within social institutions.
The medical establishment remained generally very sceptical of Hahnemann’s theories, and he in turn continued to be intensely critical of conventional medical practice. He became known as the “raging hurricane” due to his furious tirades and sarcastic critiques during lectures at Leipzig. He also antagonized contemporary pharmacists by giving only one medicine at a time, which was contrary to their (highly lucrative) practice of generally prescribing expensive mixtures of several remedies. During the 19th century, homeopathy spread rapidly across Europe to Asia and the Americas. In the US, Dr. Constantine Hering (1800–80) and Dr. James Tyler Kent (1849–1916) were responsible for popularizing the therapy and introducing new ideas and practices (see page 19). By the time of Hahnemann’s death in 1843, homeopathy was firmly established in many parts of the world, although there remained antagonism and distrust between the advocates of conventional medicine and those of homeopathy.
Between 1860 and 1890 homeopathy flourished, as many homeopathic hospitals and schools were opened, and many new remedies were proved, considerably enlarging the materia medica. Hahnemann’s followers were often doctors who defected from conventional medicine after personally experiencing treatment, including an English doctor, Frederick Quin (1799–1878), who was cured of cholera by the Camphora remedy. Quin first visited Hahnemann in Germany in 1826, and went on to introduce homeopathy in the UK, founding the first homeopathic hospital in London in 1849. During a cholera outbreak in 1854, the mortality rate at his hospital was less than half that of conventional hospitals. This information was suppressed by the national Board of Health on the grounds that “the figures would give sanction to a practice opposed to the maintenance of truth and the progress of science,” illustrating the close stranglehold the medical establishment had achieved within social institutions.
Decline & resurrection
The predominance of conventional medicine was echoed in the US. By the late 19th century, homeopathy had become a significant part of US medical practice, with about 15 percent of doctors being practicing homeopathy. During the early 20th century, however, homeopathy became largely overshadowed by conventional medicine, principally due to the rise of the American Medical Association.
The British Medical Association played a similar role in the UK, and divisions within homeopathy began to weaken the force of its message still further. Strict followers of Hahnemann and Kent’s original theories followed “classical” or “Kentian” constitutional prescribing, believing that a person’s emotional characteristics and physical symptoms should be taken into account and favoring high potencies (see page 19). Led by the British homeopath Dr. Richard Hughes (1836–1902), one strand of practitioners had, however, begun to prescribe on pathological symptoms alone, favoring low doses. This unfortunate division in homeopathic practice enabled the conventional medical establishment to gain the upper hand, and by the 1920s homeopathy had been largely suppressed in the UK.
During the late 20th century there has been a resurgence in the popularity of homeopathy, possibly due to disenchantment with aspects of conventional medicine. In many countries, particularly in central Europe, its popularity never waned to the same extent as in the UK and US, although differences in practice have evolved. Single-remedy classical prescribing is prevalent worldwide, although in Germany and France complex homeopathy or polypharmacy (the use of combination remedies or several remedies) is also popular (see page 21). In Australia there is a strong link with naturopathy, with homeopathic remedies often incorporated into naturopathic practice. In India, homeopaths have long worked successfully alongside traditional Ayurvedic medicine and conventional medicine. In the 1990s, courses in Eastern Europe pioneered by British teachers revitalized interest in homeopathy, and in Russia it continues to be implemented and developed. In South America, homeopathy is widely taught in medical schools, while in the US it is undergoing a major resurgence of popularity. According to a 1998 survey of Americans and their health, over
6 million Americans had used homeopathy in the preceding 12 months. Noting that it had been integrated into the national healthcare systems of numerous countries, including Germany, the United Kingdom, India, Pakistan, Sri Lanka, and Mexico, the World Health Organization is publishing a position paper in 2006.

The predominance of conventional medicine was echoed in the US. By the late 19th century, homeopathy had become a significant part of US medical practice, with about 15 percent of doctors being practicing homeopathy. During the early 20th century, however, homeopathy became largely overshadowed by conventional medicine, principally due to the rise of the American Medical Association.
The British Medical Association played a similar role in the UK, and divisions within homeopathy began to weaken the force of its message still further. Strict followers of Hahnemann and Kent’s original theories followed “classical” or “Kentian” constitutional prescribing, believing that a person’s emotional characteristics and physical symptoms should be taken into account and favoring high potencies (see page 19). Led by the British homeopath Dr. Richard Hughes (1836–1902), one strand of practitioners had, however, begun to prescribe on pathological symptoms alone, favoring low doses. This unfortunate division in homeopathic practice enabled the conventional medical establishment to gain the upper hand, and by the 1920s homeopathy had been largely suppressed in the UK.
During the late 20th century there has been a resurgence in the popularity of homeopathy, possibly due to disenchantment with aspects of conventional medicine. In many countries, particularly in central Europe, its popularity never waned to the same extent as in the UK and US, although differences in practice have evolved. Single-remedy classical prescribing is prevalent worldwide, although in Germany and France complex homeopathy or polypharmacy (the use of combination remedies or several remedies) is also popular (see page 21). In Australia there is a strong link with naturopathy, with homeopathic remedies often incorporated into naturopathic practice. In India, homeopaths have long worked successfully alongside traditional Ayurvedic medicine and conventional medicine. In the 1990s, courses in Eastern Europe pioneered by British teachers revitalized interest in homeopathy, and in Russia it continues to be implemented and developed. In South America, homeopathy is widely taught in medical schools, while in the US it is undergoing a major resurgence of popularity. According to a 1998 survey of Americans and their health, over
6 million Americans had used homeopathy in the preceding 12 months. Noting that it had been integrated into the national healthcare systems of numerous countries, including Germany, the United Kingdom, India, Pakistan, Sri Lanka, and Mexico, the World Health Organization is publishing a position paper in 2006.


No comments:
Post a Comment